A word of caution: I am going to be annoyingly pedantic here, but with good reason. The lighting industry has a century-long history of introducing unfamiliar technologies using familiar terminology. We later come to regret our choice of words when it becomes necessary to express precisely what we mean.
Consider, for example, the term luminance. We understand this today to mean “luminous flux per unit solid angle per unit projected source area,” which we express in candela per square meter (where a candela is one lumen per steradian), or sometimes nits. Seventy years or so ago, however, it was common to refer to “brightness,” which today is considered a subjective attribute of a point light sources (and not to be confused with “lightness,” a subjective attribute of an area light source).
The lighting industry at first distinguished between “brightness” and “photometric brightness,” but eventually accepted “luminance” as the companion of radiance. (We will not talk about “helios,” an alternative proposed and rejected in the 1940s.) In the process, it also deprecated alternate units of measurement for luminance, including stilbs, lamberts, apostilbs, skots, brils and foot-lamberts.
| Unit | Conversion Factor |
| apostilb | π |
| bril | π x 107 |
| foot-lambert | π / (0.3048)2 |
| lambert | π x 10-4 |
| skot | π x 103 |
| stilb | 10-4 |
Luminance and candela per square meter – life is so much easier when we can agree on the terminology!
Ultraviolet …
Courtesy of the current pandemic, the lighting industry is becoming all too familiar with a technology that has been in use since the 1930s – germicidal lamps emitting ultraviolet radiation that inactivate bacteria and viruses. Sadly, we are once again using familiar terminology that we will later have to deprecate in order to express what we really mean.
It does not have to be like this, however. It may be as futile an exercise as the legend of King Canute the Great ordering the tide to stop, but we can at least examine what terminology we should be using when discussing ultraviolet radiation as a means of disinfection.
We begin with the term ultraviolet, which designates a region of the electromagnetic spectrum beyond that of visible light with wavelengths of approximately 400 nm to 700 nm. The ultraviolet region is divided by the International Lighting Commission (CIE) into three subregions:
| UV-A | 315 nm – 400 nm |
| UV-B | 280 nm – 315 nm |
| UV-C | 100 nm – 280 nm |
Here, however, is the point: “ultraviolet” is an adjective. It makes as much sense to refer to “ultraviolet” as it does to refer to “blue” – blue what? Just as we invariably refer to “blue light” in lighting design, we should refer to ultraviolet radiation. (For the record, light is “the natural agent that stimulates sight and makes things visible”; all else – including light – is electromagnetic radiation.)
Germicidal
From here, we move on to the term germicidal. This refers to the effect of UV radiation on pathogens, including viruses, bacteria, and fungi. Ultraviolet photons have enough energy to disrupt the DNA and RNA of bacteria and fungal cells, preventing the organisms from reproducing and thus inactivating them; eventually, they die. Viruses are not technically alive, but in disrupting their genetic code, the UV radiation prevents them from invading living cells and replicating, and thus inactivates them as well.
Unfortunately, this has led to the increasingly popular term germicidal UV, abbreviated GUV. Respecting the previous argument, a better term is ultraviolet germicidal irradiation (UVGI). This has a long history of use in the ultraviolet disinfection community, and the lighting industry should respect it as being unambiguous.
Luminaires
For anyone in the lighting industry, a product that emits visible light is a luminaire. … except that ultraviolet radiation is not light.
There are several types of ultraviolet radiation sources:
Low-pressure mercury-vapor arc lamps
These are basically linear or compact fluorescent lamps without phosphor coatings to convert ultraviolet radiation into visible light, and fused quartz or “soft” glass tubes that are transparent to UV-C radiation. They emit essentially monochromatic UV-C radiation with a wavelength of 254 nm. (The tubes are usually designed to block 185 nm radiation, which can generate toxic ozone.) They are typically used for “upper-room” air disinfection (CIE 2003), HVAC air ducts, and mobile ultraviolet disinfection platforms and robots.
Medium-pressure mercury-vapor arc lamps
These are similar to high-intensity discharge (HID) lamps, but feature broadband radiation centered around 250 nm. They are mostly used for water disinfection purposes.
Pulsed xenon lamps
These are basically high-power electronic flash lamps which emit intense broadband radiation across the entire ultraviolet spectrum with a peak near 230 nm. They are commonly used with mobile disinfection platforms in hospitals.
Excimer lamps
Krypton-chlorine (KrCl*) excimer lamps emit mostly ultraviolet radiation with a peak wavelength of 222 nm, and are being explored as a safer alternative to low-pressure mercury-vapor arc lamps.
Microplasma emitters
Microplasma emitters are based on the essentially the same technology formerly used to produce plasma television screens, but are designed to emit ultraviolet radiation with a peak wavelength of 222 nm.
UV-LEDs
Ultraviolet-emitting LEDs are becoming increasing available, although to date with exceedingly low radiant efficiencies of one to four percent and peak wavelengths no shorter than 265 nm for commercial devices. However, the roadmap for the development of UV-C LEDs promises much greater efficiencies in the foreseeable future (Krames 2020).
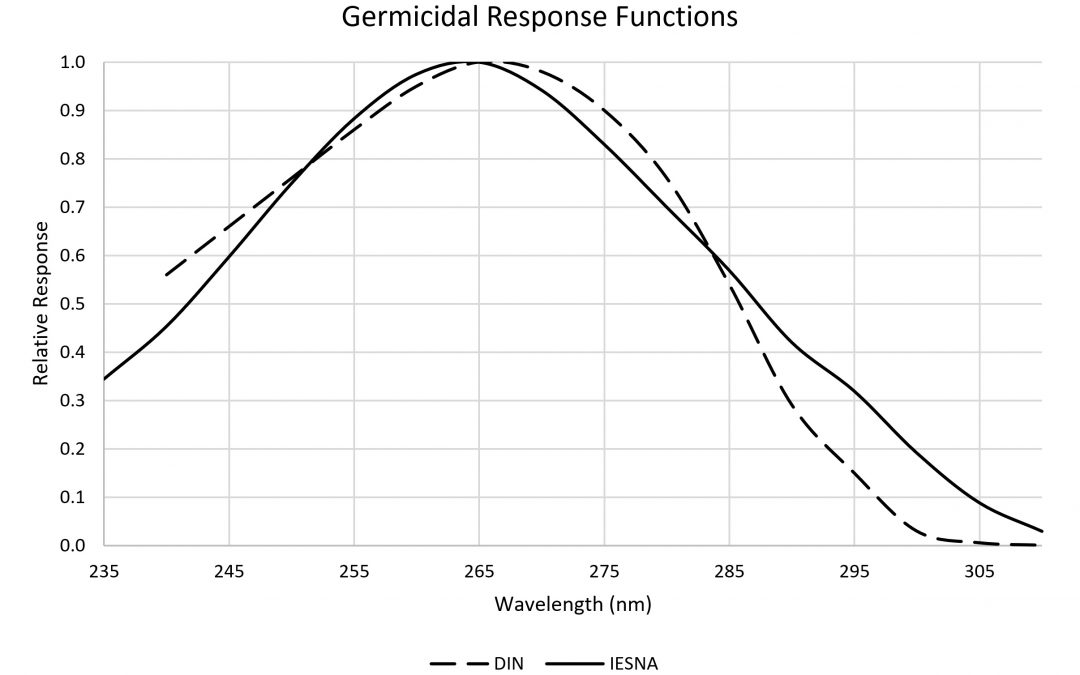
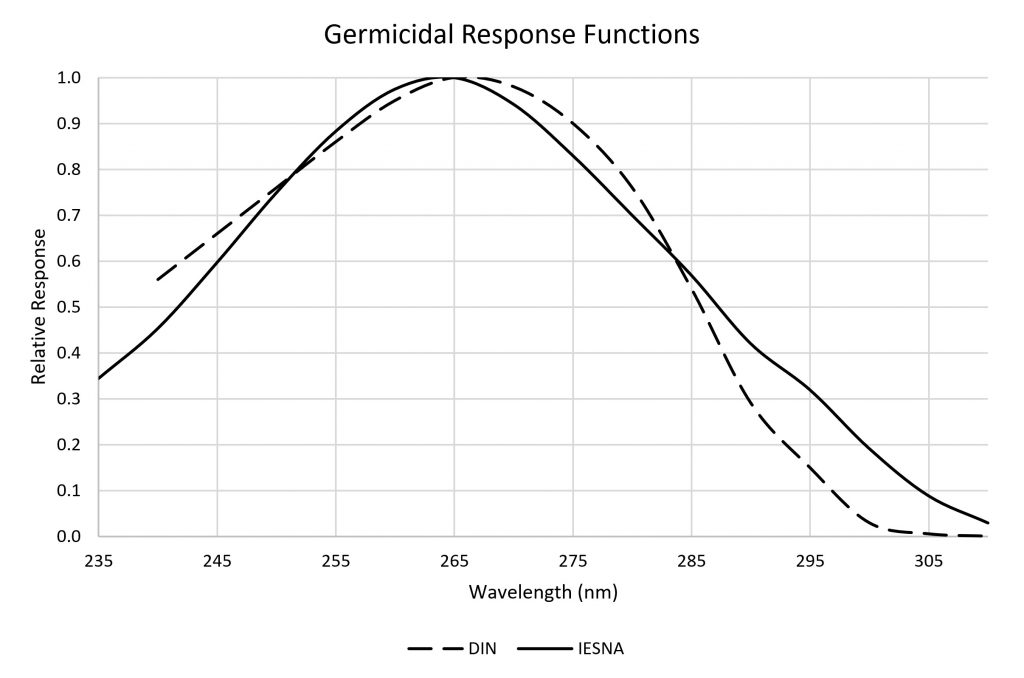
For germicidal purposes, the optimal wavelength for disrupting the DNA of pathogens is 265 nm (Figure 1). Once again, however, this is electromagnetic radiation and not light. It may therefore be preferable to refer to UVGI sources rather than “luminaires.”
Radiometry
This should be an easy one. For proper UVGI systems design, we will need to know the intensity distribution of the UVGI sources, just like we have luminous intensity distributions for luminaires and photometric data reports.
Measuring these characteristics in the laboratory is not easy. Integrating spheres measuring two meters or more in diameter are often used to measure the luminous flux generated by luminaires, but the typical barium sulphate (BaSO4) coating is not sufficiently reflective for ultraviolet radiation measurements. Microstructured polytetrafluoroethylene (PTFE), perhaps best known as Labsphere Inc.’s diffuse reflectance standard Spectralon, has acceptable reflectance (> 95 percent at 250 nm), but it must be machined rather than applied as a coating.
Regardless, what is being measured is the radiant intensity distribution of the UVGI sources, with corresponding radiometric data reports. This further implies that these reports should be based on the ANSI/IES TM-33-18 luminaire optical data document specification rather than ANSI/IES LM-63-19 (and earlier editions) and EULUMDAT file formats, which are specific to photometric data (IES 2018). (The Italian UNI 11733:2019 standard is a mirror document to ANSI/IES TM-33-18.) This document specification was developed specifically with ultraviolet radiometry in mind.
More generally, we should always use radiometric units when referring to the performance of UVGI systems:
| Photometric | Radiometric |
| Illuminance (lm/m2) | Irradiance (μW/cm2) |
| Luminous intensity (cd) | Radiant intensity (μW/sr) |
| Luminance (cd/m2) | Radiance (μW/sr-cm2) |
| — | Radiant fluence (mJ/cm2) |
The International Bureau of Weights and Measurements defines radiometric measures in terms of watts, meters, and steradians, but UVGI systems typically express measurements in microwatts (μW) and square centimeters (cm2) for convenience (BIPM 2019).
Radiant Dose
If, as a professional lighting designer, you did a double take on the term radiant fluence, it is understandable – what is this? ANSI/IES RP-16-17 (ANSI 2017) defines “radiant fluence” as “the omnidirectional radiant energy externally incident on an elementary sphere per unit cross-sectional area in time Δt,” or more succinctly:

where dω is the differential solid angle, da is the cross-sectional area of the sphere, and Δt is the exposure time. (I warned you that I was going to be annoyingly pedantic.)
Fortunately, this metric is much simpler conceptually than its formal definition implies, and it is crucial to an understanding of UVGI system performance.
The SARS-CoV-2 virus is transmitted primarily by respiratory droplets and aerosols that are generated by the simple acts of breathing, talking, sneezing, coughing and singing. The same is true, however, for many other viruses, bacteria, and fungi, including those responsible for the common cold, influenza, measles, chickenpox, and tuberculosis. Respiratory droplets, which are typically larger than 5 μm and consist mostly of water, fall to the ground rapidly after being produced. Aerosols, on the other hand, are relatively dry and may persist in the air for several hours.
Imagine then a droplet or aerosol as a transparent sphere holding the viruses or bacteria in solution. Seen from any direction, the cross-sectional area is defined by the equation for the area of a circle: π x r2, where r is the sphere radius.
Now think of a parallel beam of ultraviolet radiation in this direction. The beam has a measurable radiance L that is expressed in microwatts per steradian per square centimeter (μW/sr-cm2). Conceptually, it is the radiant power of the ultraviolet photons passing through the transparent sphere in the given direction at a specific moment in time.
If we sum the beam radiance for all possible directions, we have the irradiance of the sphere. We can make the diameter of the sphere infinitesimally small, in which case we have the spherical irradiance (aka the fluence rate) of the elementary sphere at a point in free space, measured in microwatts per square centimeter (μW/cm2).
It is not however the irradiance that is important for germicidal action, but rather the radiant dose or fluence. The aerosol particle may drift through the air and thus be exposed to varying levels of spherical irradiance. The longer the particle is exposed to radiation, however, the more likely it is that a UV photon will intersect the DNA or RNA of a virus (which typically has a diameter of less than 100 nanometers) and disrupt it.
Fluence then is the spherical irradiance (measured in μW/cm2) of the particle integrated (i.e., summed) over time (measured in seconds). One joule (energy) is one watt (power) times one second. For UVGI purposes is typically expressed in millijoules per square centimeter (mJ/cm2).
Fluence is defined specifically for aerosols (and more generally points in free space), but the concept of radiant dose also applies to the irradiation of surfaces. For a uniform distribution of radiance (i.e., equal in all directions), the irradiance of a surface is 1 / π times that of spherical irradiance without the surface at that point.
Choosing Radiant Dose
When the UV dose results in a 90 percent disinfection (10 percent survival), it is referred to as D90. For UVGI applications where higher disinfection rates are needed, D99 (i.e., 99 percent disinfection) is often used. To completely disinfect a surgical tool, it is common to expect 99.9999 percent disinfection. There may still be a few active viruses or bacteria that remain, but their density is too low to achieve an infection or replicate in a colony.
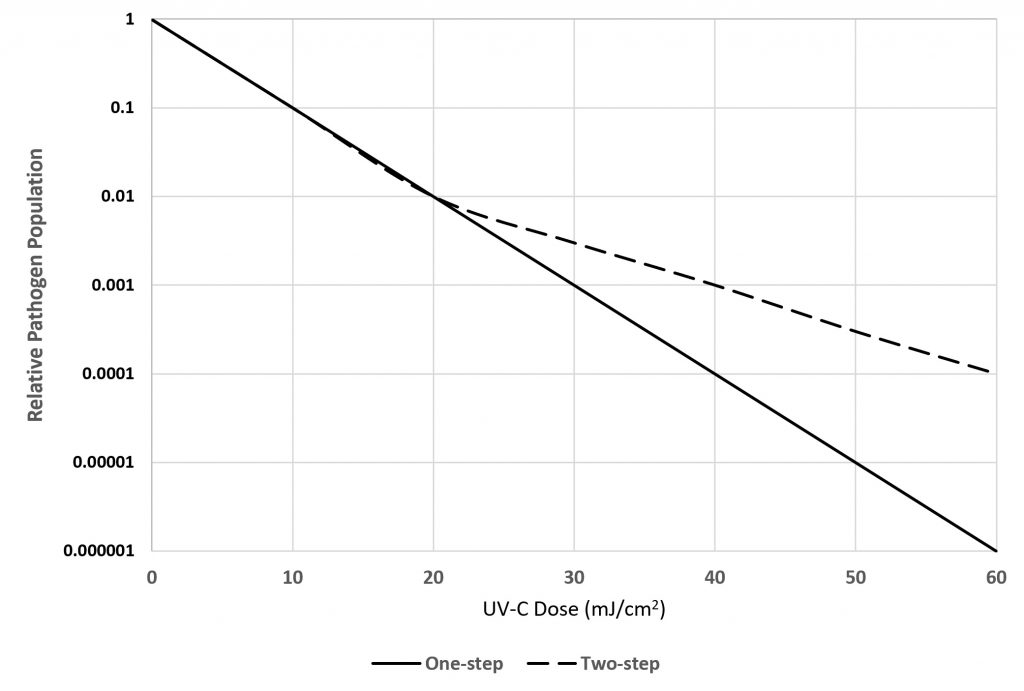
The decrease in survival with larger UV doses is exponential – if 10 mJ/cm2 results in 90 percent disinfection, 20 mJ/cm2 results in 99 percent, 30 mJ/cm2 in 99.9 percent, and so on. This is an example of exponential decay, and so it is more convenient to refer to the disinfection in logarithmic units: D90 is log-1 , D99 is log-2, and so on to log-6 for complete disinfection.
There are however complications in determining an appropriate UV dose for inactivating pathogens. Table 4 (adapted from Kowalski 2009) presents the average radiant doses required to achieve D90 disinfection for pathogens:
| Pathogen | Type | Water | Surface | Air – Low RH | Air – High RH |
| Bacteria | Vegetative | 2.7 | 1.6 | 0.6 | 3.1 |
| Bacteria | Spores | 16.0 | 12.6 | 9.0 | 8.9 |
| Fungi | Vegetative | 22.9 | 32.9 | 2.3 | — |
| Fungi | Spores | 25.1 | 29.2 | 31.5 | 48.8 |
| Viruses | All | 4.0 | 7.3 | 0.6 | 0.8 |
(RH – relative humidity, expressed in percent.)
The first complication is that the pathogen species and its environment matters. Hundreds of studies have reported on the susceptibility of many different pathogen species to either monochromatic (254 nm) or broadband UV irradiation, where the pathogens are: a) suspended in water; b) cultured on a growth medium on a surface (e.g., a Petri dish); or c) suspended in airborne droplets or aerosol particles of various sizes. As shown in the table, the relative humidity of the air can have a very significant effect on vegetative bacteria (but not viruses).
The second complication is that Table 4 represents the average dose for D90 disinfection. Depending on the pathogen species and environment, the required dose can vary by a factor of 100 or more from these averages. Designing a UVGI system with an average radiant dose does not guarantee protection from specific pathogens. The choice of narrowband versus broadband radiation sources also matters, especially for bacteria.
The third complication is that once D90 disinfection has been achieved, it is often the case that the surviving 10 percent of the population is an order of magnitude more resistant to UV irradiation. For example, if it takes 10 mJ/cm2 to achieve D90 disinfection, it may take 40 mJ/cm2 to achieve D99 disinfection.. As shown in Figure 2, such pathogens are said to have a “two-step” rare constant for their susceptibility to UV-C radiation.
A fourth complication is that when vegetative bacteria and fungi have been exposed to monochromatic UV radiation as a means of disinfection, subsequent exposure to visible light may enable the “killed” cells to repair their DNA and recolonize, thereby increasing their survival rate by 10 to 100 times, especially if the pathogens are suspended in water or present on surfaces in the presence of high relative humidity. (Viruses do not seem to have the complexity needed to effect self-repair of their DNA.) This may be a concern if, for example, the exposed surfaces of a hospital room are decontaminated with a mobile UV disinfection robot, but the room is flooded with direct sunlight thereafter.
A fifth and final complication is that once a surface has been infected with respiratory droplets, any bacteria may find sufficient resources to begin colonizing the surface. The surface may be continuously irradiated by, for example, UV‑C radiation from a microplasma emitter or UV-LED array, but if the irradiance is too low, the surface may not achieve even D90 decontamination, regardless of the exposure time.
Summary
There is admittedly a considerable amount of information here that extends beyond the bounds of ultraviolet radiation terminology. It is needed, however, to put the terminology used for decades by the ultraviolet disinfection community into context. Ultraviolet radiation is not visible light, and so the lighting community needs to both understand and respect the terminology when adopting UVGI system design practices for building safety and human health. If we do not use the correct terminology, we risk (and deserve) a plague of apostilbs, brils, lamberts, skots and other annoyances later down the road.
References
BIPM. 2019. The International System of Units (SI), 9th Edition (https://www.bipm.org/utils/common/pdf/si-brochure/SI-Brochure-9-EN.pdf).
CIE. 2003. CIE 155:2003, Ultraviolet air Disinfection. Vienna, Austria: CIE Central Bureau.
CIE. Undated. CIE International Lighting Vocabulary (http://eilv.cie.co.at/termlist).
Kowalski, W. 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for air and Surface Disinfection. Heidelberg, Germany: Springer.
IES. 2017. ANSI/IES RP-16-17, Nomenclature and Definitions for Illuminating Engineering (https://www.ies.org/standards/definitions).
IES. 2018. ANSI/IES TM-33-18, Standard for the Electronic Transfer of Luminaire Optical Data. New York, NY: Illuminating Engineering Society.
Krames, M. 2020. “The Rise of UV-C LEDs,” LEDs Magazine 125:36-39.